GMPPB Variant Identified in 3 Consanguineous Iranian Families with LGMD Through Exome Sequencing
- Ruth Wright
- Sep 16, 2020
- 7 min read
Updated: Mar 29, 2021
The dystrophin-glycoprotein complex is responsible for attachment of muscle fibres to the extracellular matrix and is vital for muscle stability and integrity. Mutations affecting the complex result in muscle fibres that are vulnerable to damage caused by normal repetitive contraction and relaxation. The aim of my undergraduate research project was to identify the genetic cause within 3 families presenting with Limb-Girdle Muscular Dystrophy (LGMD); a rare type of muscular dystrophy.
The dystrophin-glycoprotein complex (DGC) consists of the dystrophin protein linked to the glycoprotein complex which, is made up of several proteins: sarcoglycans, sarcospans and an alpha- and beta-dystroglycan (1) . The beta-subunit has a transmembrane domain within the muscle fibre sarcolemma, while the alpha-subunit binds to laminin and forms an anchor with the surrounding basal membrane. This is illustrated in the image below.

Alpha-dystroglycan undergoes significant post-transcriptional modification, crucial to the laminin-binding capacity of the alpha-dystroglycan subunit. Understandably, this is a highly regulated process and mutations affecting glycosylation would disrupt laminin binding affinity of the whole glycoprotein complex. Affected muscle fibres show increased muscular vulnerability to damage from normal mechanical stress, resulting in progressive muscle disorders. Such disorders are known as dystroglycanopathies.
Dystroglycanopathies are highly heterogeneous in both genetic cause (genotype) and clinical manifestations (phenotype) with a wide spectrum of severity. On the one side, patients present with congenital abnormalities to the brain, eye and muscle e.g. Walker-Warburg syndrome, muscle-eye-brain disease and Fukuyama muscle dystrophy. Whereas, milder cases present without brain or eye abnormalities e.g. LGMD, with onset sometimes late into adulthood.
The problem faced by clinicians and researchers when trying to diagnose patients with dystroglycanopathies remains, the degree of heterogeneity and the degree of phenotypic overlap. This makes selecting appropriate genetic tests particularly difficult when solely looking at clinical symptoms. What’s more, 20-50% of patients from large cohorts do not have mutations in any of the genes currently known to be associated with dystroglycanopathies. Consequently, a significant number of patients remain undiagnosed.
Purpose
The aim for this project was to identify the underlying causal mutation within 3 separate consanguineous families presenting with Limb-Girdle Muscular Dystrophy (LGMD). Considering the extensive heterogeneity in both clinical and genetic presentation of dystroglycanopathies, a genetic approach was taken applying whole exome sequencing and variant prioritisation. Sanger sequencing and co-segregation analysis was performed on the 3 probands and any available family members to confirm the presence of likely mutations. Further diagnostic weight was provided by homozygosity mapping, pathogenicity classification and amino acid signal-to-noise analysis.
Whole Exome Sequencing and Prioritisation
Exome sequencing was performed on blood samples obtained from 3 individuals (probands) from 3 consanguineous families of Iranian decent, presenting with LGMD. The family pedigrees are illustrated in the figure with probands indicated by an arrow. Approximately 250,000 mutations were obtained for each proband but, after removing mutations highly unlikely to be pathogenic, less than 10 mutations remained for each proband. Of the remaining mutations only the C>T mutation at position 308 (c.C308T:p.P103L) in the GMPPB gene had been previously associated with dystroglycanopathies.

Homozygosity mapping
Under the assumption that the disease phenotype is following autosomal recessive inheritance, the probands’ were analysed for regions of homozygosity which would indicate genes likely to be identical-by-descent. In other words, should a particular mutation be the cause of a patients LGMD, then it would be expected that the DNA sequence surrounding that mutation would be the same as members of the patients family; a result of recent common ancestry.
Initially, this analysis did not find a region of homozygosity however, upon more thorough investigation of the WES data from each proband, a region of homozygosity was identified that was first missed. This appeared to be the result of a small region of heterogeneity isolated to the MST1 gene occurring directly before the GMPPB variant in all 3 probands. A history of consanguinity within a population has been found to increase the percentage of homozygous autosomal regions by 2-3% (2,3) and in addition to the fact that the heterozygous region was isolated to MST1 gene in all 3 families, it suggests that the heterozygous region is an artifact of sequence-read misalignment error in the WES technology.
Sanger Sequencing + Co-segregation
Sanger sequencing results from the affected individuals confirmed the presence of the homozygous GMPPB variant c.C308T:p.P103L in all probands. Unfortunately, co-segregation with disease was only identified in family B and lack of available samples from any relative prevented co-segregation analysis from being performed at all on family C.
ACMG Classification
Classification of a variant’s pathogenicity is important for its application in a clinical setting. A clinical laboratory classification of a variant as ‘pathogenic’ can be taken by health-care providers as ‘actionable’ thus resulting in changes to a patient’s treatment, surveillance and/or removal of management entirely. Therefore, it is important when classifying the pathogenicity of a variant to compile evidence from various sources to refine diagnostic weight.
The American Collage of Medical Genetics and Genomics (ACMG) guidelines for variant classification (4) aims to determine, from an aggregate of evidence, whether a variant in a gene with a definitive role in a mendelian disorder is pathogenic for that specific disorder; in this case dystroglycanopathies. It is a stringent classification system, with the overall goal of decreasing the number of variants being classified as causative without substantial evidence to back it up. The ACMG guidelines classified the c.C308T:p.P103L GMPPB variant as ‘likely pathogenic’ but, recommend that for all sequence variants classified as either ‘pathogenetic’ or ‘likely pathogenic’ for further confirmation studies should be conducted. These may include, re-extraction and re-testing of the sample, testing parents, re-sequencing the area of interest, restriction enzyme digestion, or use of alternative genotyping technologies (4).
Amino-Acid Signal-to-Noise Analysis
Amino-acid signal-to-noise analysis was used to refine the diagnostic weight of the ‘likely pathogenic’ classification of the GMPPB variant c.C308T:p.P103L. It was able to identify 2 larger and 1 smaller ‘peak of pathogenicity’ along the primary structure of GMPPB. Unfortunately, the c.C308T:p.P103L variant did not fall within one of these peaks, meaning there is low signal-to-noise at the loci of the variant and therefore may be less likely to be disease-causing. If the variant had fallen into one of these ‘peaks of pathogenicity’, then it would have suggested that variant is disease-causing. It is important to note that the low signal-to-noise at c.C308T:p.P103L does not, in itself, disprove the variant’s pathogenicity. Rather, it is another point of evidence that must be considered in the context of all accumulated findings.

So What is GMPPB?
GDP-mannose pyrophosphorylase B (GMPPB) is a transferase protein involved in the production of dolichol phosphate mannose, a substrate required for the creation of O-mannosylated (O-Man) glycans (see diagram below). These O-Man glycans have been linked to the laminin-binding property of alpha-dystroglycan (5) and hence the disruptions of proper O-mannosylation understandably results in reduced laminin binding to the DGC.

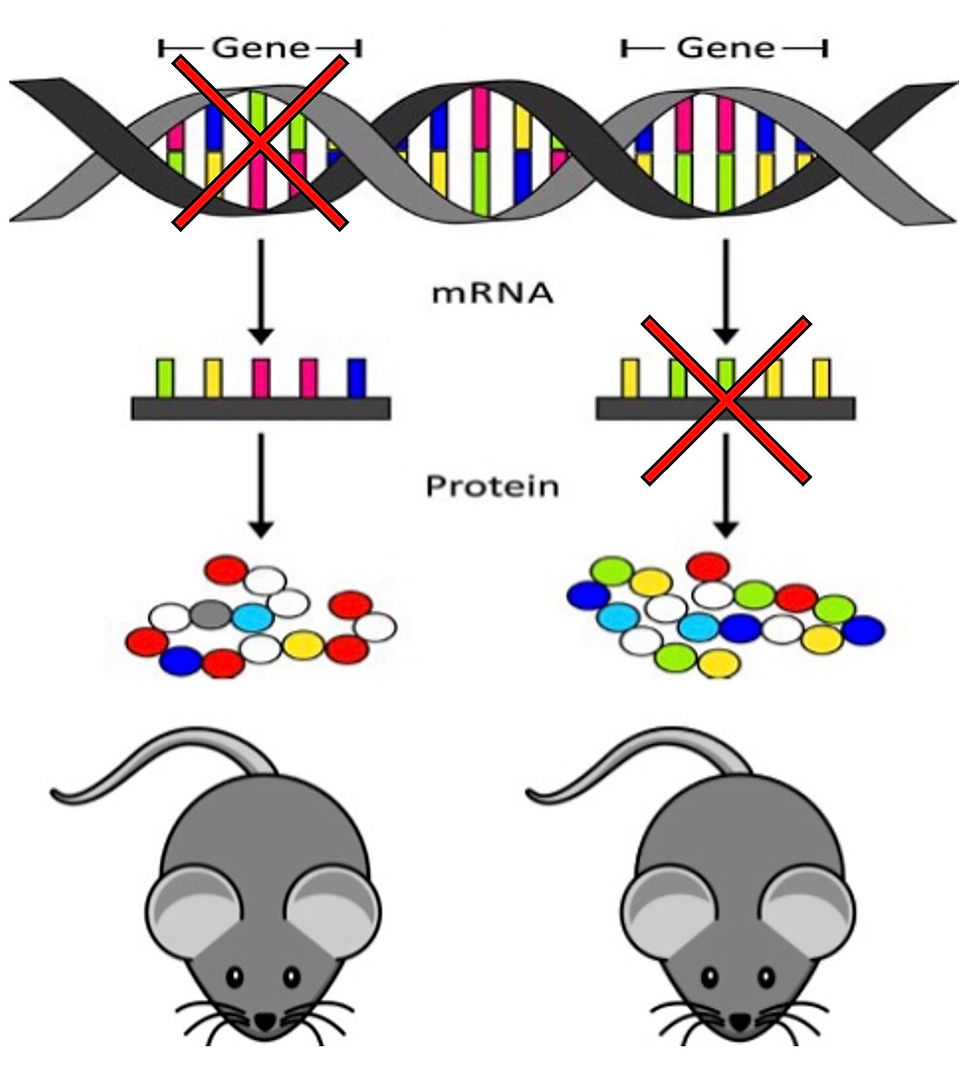
Research on zebrafish lacking GMPPB found structural muscular, brain, and eye abnormalities, along with a hinderance to both mobility and glycosylation of alpha-dystroglycan which reflects the human phenotype (6). One possible hypothesis as to why GMPPB variants present with a wide spectrum of clinical manifestations previously proposed (7), is that due to GMPPB’s ubiquitous expression and its involvement in several different proteins. Another hypothesis proposed is that aberrant GMPPB function could ultimately hinder POMT function and thus result in different knock on effects depending on the tissue specific POMT expression.
Further Research
Due to the limited time frame of this project, a significant amount of work is still needed to draw any definite conclusions. This could include, the recruitment of more consanguineous families with LGMD. This may offer more probands with GMPPB causal mutation, dealing with available samples from several relatives with and without LGMD. Furthermore, gene expression (transcriptome) analysis could be performed to observe the effect potentially causal mutation may have on the expression. Finally, functional experiments are required to assess the biological consequences and prove pathogenicity of novel variants/genes.
Zebrafish (ZF) are already a recognised pre-clinical animal model and are a good option for loss-of-function experiments. Morphalino oligonucleotides could be used to target ZF orthologues (genes in different species with shared ancestral backgrounds and therefore shared function). These morphant ZF can then be injected with a normal version of a gene which should in theory reduce the severity of symptoms and act as supporting evidence that the phenotype is specific to the gene of interest. Morphalino ZF could also be screened against drug libraries to potentially identify drug/pathways that may be applied to later therapeutic options.
So, Where Does This Leave Us?
LGMD, unfortunately, remains another disease without an available treatment even for those patients for whom a genetic diagnosis has been made. However, a genetic diagnosis still offers substantial peace of mind and as well as avenues for family planning and experimental treatment. Hopefully, future investigation of these 3 families and others like them will in time bring better treatment options and with it an overall better quality of life to those suffering with LGMD.
This project would not have been possible without the expertise and encouragement from my amazing supervisor Dr. Yalda Jamshidi. Yalda’s research group studies the impact of variation in the genome on disease susceptibility and investigate the role DNA mutations have on development and disease.
References:
Bouchet-Séraphin C, Vuillaumier-Barrot S, Seta N. Dystroglycanopathies: about numerous genes involved in glycosylation of one single glycoprotein. J Neuromuscul Dis. 2015;2:27–38.
Zimon M. et al. Unraveling the genetic landscape of autosomal recessive Charcot-Marie-Tooth neuropathies using a homozygosity mapping approach. Neurogenetics 2015;16:33–42.
Woods CG, Cox J, Springell K, Hampshire DJ, Mohamed MD, McKibbin M, Stern R, Raymond FL, Sandford R, Malik SS, Karbani G, Ahmed M, Bond J, Clayton D, Inglehearn CF. Quantification of homozygosity in consanguineous individuals with autosomal recessive disease. Am J Hum Genet. 2006;78:889–896.
Richards S, Aziz N, Bale S, Bick D, Das S, Gastier-Foster J et al. Standards and guidelines for the interpretation of sequence variants: a joint consensus recommendation of the American College of Medical Genetics and Genomics and the Association for Molecular Pathology. Genetics in Medicine. 2015;17(5):405-423.
Michele D, Campbell K. Dystrophin-Glycoprotein Complex: Post-translational Processing and Dystroglycan Function. Journal of Biological Chemistry. 2003;278(18):15457-15460.
Carss KJ, Stevens E, Foley AR, Cirak S, Riemersma M, Torelli S, et al. Mutations in GDP-mannose pyrophosphorylase B cause congenital and limb-girdle muscular dystrophies associated with hypoglycosylation of α-dystroglycan. Am J Hum Genet. 2013;93:29–41. doi: 10.1016/j.ajhg.2013.05.009.
Belaya K, Rodríguez Cruz PM, Liu WW, Maxwell S, McGowan S, Farrugia ME, et al. Mutations in GMPPB cause congenital myasthenic syndrome and bridge myasthenic disorders with dystroglycanopathies. Brain. 2015;138(Pt 9):2493–2504. doi: 10.1093/brain/awv185.



Comments